Osteopenia, Osteoporosis, Osteonecrosis
It’s estimated that between 1 and 3 women, and 1 in 12 men over the age 50 worldwide, suffer from the bone weakening disease known as osteoporosis. Osteoporosis occurs when there is an imbalance between bone reabsorption (osteoclast cells) and bone formation (osteoblast cells). Bone is a living tissue that undergoes constant transformation. At any given moment there are from 1-10 million sites where small segments of old bone are being broken-down (reabsorbed) and new bone is being laid down to replace it. When more old bone is destroyed than new bone laid down, bone loss occurs.

Prior to 1974, surveys showed that 77 percent of Americans had never heard of osteoporosis. In 1992 in an effort to reduce the incidence of osteoporosis fractures, The World Health Organization (WHO) held an international conference. Aided by new bone testing technology experts at the conference, which was sponsored by two large drug companies and a drug-company foundation, were charged with determining the normal bone density mass. The researchers turned to an analysis of women in Rochester, Minnesota, which showed that 16 percent of post-menopausal women in that city would sustain a hip fracture in their lifetime. Looking at years of bone-density scores, the WHO found that 16 percent of post-menopause women had bone –density readings of -2.5 or worse. So, under the new definition, anyone with a spinal fracture or a -2.5 T-score (bone density score), or worse, had osteoporosis. The committee went further and decided that scores between -1 and -2.5 were the boundaries of a new condition called osteopenia, or low bone mass.
In a single conference, one disease, osteoporosis, had been expanded from an elderly person with a fracture to anyone with a -2.5 T score. And another condition, osteopenia, was created.
Critics for the criteria for the diagnosis of osteoporosis began to emerge almost immediately. One rationally minded expert disagreed with the idea that randomized numbers could determine who did and who didn’t have a disease. Dr. Steven Cummings one of the world’s leading osteoporosis experts declared, “What patients had were measurements, not disease.” This is analogous to the idea that everyone with elevated cholesterol has heart disease.
Many have continued to argue that the concept of peak bone mass has been oversimplified. Peak bone mass can vary as much as 100% in women of the same age from different cultures. And peak bone mass seems to have minimal affect on fracture risk: for instance, Asian women have a lower bone mass than Western women but a lower fracture rate.
Never the less, once considered a rare disease associated with old ladies with a “dowagers hump,” osteoporosis has now become an epidemic with “experts” warning that half of all post-menopausal women are at risk.
How did osteoporosis go from a rare but serious disease to an epidemic that strikes fear in every middle-aged woman in America? One word, Merck.

Pharmaceutical giant Merck shrewdly launched an aggressive campaign to educate the public and their doctors that osteoporosis and the new disease known as osteopenia were now treatable with their new drug, Fosamax. Merck promoted portable bone-measuring devices that doctors could use in their offices. When Merck started, there were 750 dual-energy x-ray absorptiometry (DXA or DEXA) bone-measuring devices in the United States. Four years later, there were over 10,000 machines, which tested over 3.5 million people a year! The goal wasn’t to sell the drug to the elderly who actually had osteoporosis but to make it a primary care drug for the 40 million post-menopausal women. With sales of bisphosphonates approaching 5 billion dollars a year, the propaganda for these drugs now rival another once overly hyped drug for osteoporosis prevention, Premarin. These drugs were the number one prescribed drug therapy in America in 2001.
Of course the results of The Women’s Health Initiative in 2002, which showed that while estrogen did reduce bone loss, it also increased the risk of breast cancer, blood clots, heart attack, and stroke sort of put a damper on estrogen therapy, to say the least. That same year there was an initial 80 percent drop in hormone therapy drug sales.
Sales of Fosamax and other bisphosphonates (Actonel and Boniva) increased 32 percent after the WHI study came out. These drugs do increase bone mass. However, they are also associated with numerous side effects including upper gastrointestinal pain and erosion, esophagitis, ulcers, skin rash, diffuse bone pain, and osteonecrosis (bone death) of the jaw.
Previously, bisphosphonates had been used in laundry soaps, fertilizer, and anticorrosives for the textile and oil industries. A 1993 report discovered that a small percentage of bisphosphonates users experienced serious eye problems that could lead to blindness. Merck’s clinical trial showed that as many as 33 percent of the participants reported blurred vision. Even more troubling, another study quoted on April 4, 2006, by United Press International, found more than 2,400 patients who were taking the injected form of bisphosphonates had suffered bone damage to their jaws since 2001. In addition to the 2,400 patients who were taking the injected form, the study found 120 patients taking the oral form of the drug who had been stricken with such incapacitating bone, joint, or muscle pain that some became bedridden and others required walkers, crutches or wheelchairs. We’ve uncovered about 1,000 patients (with jaw necrosis) in the past six to nine months alone, so the magnitude of the problem is just starting to be recognized,” Kenneth Hargreaves, of the University of Texas, reported to the Los Angeles Times. And we need to consider that the FDA estimates that only 10 percent of adverse drug events are ever reported. Rats given high doses developed thyroid and adrenal tumors. Fosamax also causes deficiencies of calcium, magnesium and vitamin D, all essential for the bone-building process.
Another commonly prescribed osteoporosis drug, Evista, is a selective estrogen receptor modulator. It is promoted as a safe way to increase estrogen without any of the side effects of hormone replacement therapy. But, of course there are side effects, which include hot flashes, leg cramps, flu-like symptoms, blood clots (heart attack and stroke), and peripheral edema.
The osteoporosis propaganda campaign has caused women to believe that they must take a drug to prevent being bent over with spinal fractures or succumbing to a life threatening hip fracture. No doubt, the prospect of having a broken bone due to osteoporosis is quite frightening. However the average age of hip fractures for a woman is 79. The lifetime risk of hip fracture for a white American female age 50 or older is 17.5 percent. Over a lifetime the risk for a vertebral fracture for this same group is estimated at 15 percent. Certainly these percentages should make us pause and take note. However, leading bone expert, and author of Better Bones, Better Body, Susan E. Brown, PhD, states: “Osteoporosis by itself does not cause bone fractures. This is documented simply by the fact that half of the population with thin osteoporitic bones in fact never fracture.” It is important to know that over 90 percent of hip fractures occur from falls, not weak bones. Falls cause fractures, not weak and crumbling osteoporitic bones.
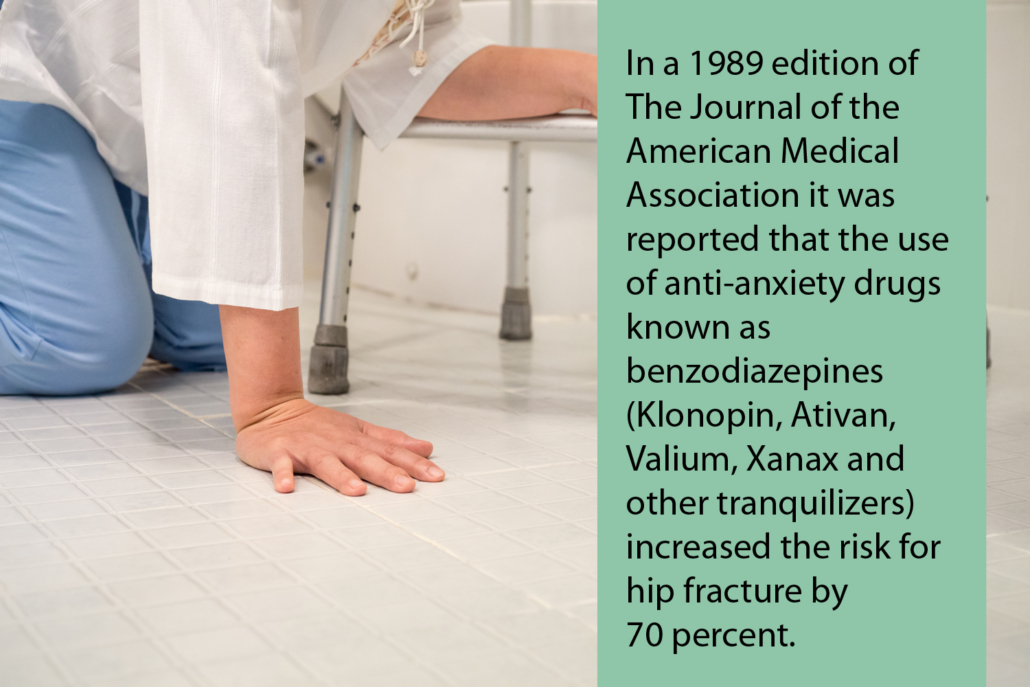
Bone does not fracture due to thinness alone. A 1995 edition of the New England Journal of Medicine reported that in 65-year-old women with no previous history of a hip fracture, a number of other factors were more significant than bone density in predicting fractures, such as tranquilizer and sleeping pill use, poor coordination, poor vision and depth perception, low blood pressure, and lack of muscle strength.
Dr. Mark Helfand, a member of the U.S. National Institute of Health osteoporosis consensus panel comments: “I think even people who agree that osteoporosis is a serious health problem can still say it is being hyped. It is hyped. Most of what you can do to prevent osteoporosis later in life has nothing to do with getting a test or taking a drug.”
Drug therapy may be appropriate for those with advanced bone loss, especially since 20 percent of those age seventy or older with hip fractures never recover. But before starting on potentially dangerous drug therapy at the first sign of bone loss, patients need to be educated on the role nutrition plays in ensuring optimal bone health. There are at least 18 key bone-building nutrients essential for optimal bone health. Vitamins D, E, C, B12, K, folic acid, and minerals including boron, calcium, magnesium, copper, and zinc are needed for proper bone production and restoration. All of these nutrients have been shown to reduce and in some cases restore optimal bone mass.
I think patients would be better served by using prevention and optimal nutrition instead of taking a bone-eating prescription.  While I don’t agree with the propaganda associated with osteoporosis, especially that every perimenopause and postmenopausal woman needs to be taking bisphosphanates (Fosamax, Actonel, Boniva), osteoporosis is an all-too-common condition that can be life-threatening for many elderly Americans. However, the majority of osteoporosis cases could have been prevented. This disease is similar in nature to so many other “Western diseases,” all associated with poor nutrition and health-robbing lifestyles. Bone is a living tissue that is constantly being broken down and rebuilt. Bone health is dependent on routine weight-bearing exercise, healthy habits (no smoking, moderate alcohol, caffeine, and sugar consumption, etc.) and an intricate interplay of over a dozen nutrients.
While I don’t agree with the propaganda associated with osteoporosis, especially that every perimenopause and postmenopausal woman needs to be taking bisphosphanates (Fosamax, Actonel, Boniva), osteoporosis is an all-too-common condition that can be life-threatening for many elderly Americans. However, the majority of osteoporosis cases could have been prevented. This disease is similar in nature to so many other “Western diseases,” all associated with poor nutrition and health-robbing lifestyles. Bone is a living tissue that is constantly being broken down and rebuilt. Bone health is dependent on routine weight-bearing exercise, healthy habits (no smoking, moderate alcohol, caffeine, and sugar consumption, etc.) and an intricate interplay of over a dozen nutrients.
Children raised on a diet of Fruit Loops, “Lunchables,” soft drinks, and “Happy Meals,” don’t get the essential nutrients needed for optimal health. Few 12 to 19 year-olds consume the recommended amounts of certain nutrients. Adolescent girls consume only 14% of the Recommended Dietary Allowance (RDA) for calcium, 31% of vitamin A, and only 18% of the RDA for magnesium. Adolescent boys aren’t much better. Children consuming a typical nutrient-deficient Western diet are setting the stage for the onset of osteoporosis.
Soft drinks now make up one third of an adolescent’s daily beverage intake. This depletes bone-building calcium. Ninth and tenth grade girls who drink sodas have three times the risk of bone fractures compared with those who don’t drink carbonated beverages.
Fifty-six percent of 8-year-olds down soft drinks daily, and a third of teenage boys consume three or more cans of soda a day. The average teenager is getting 20 teaspoons of sugar a day from soft drinks alone. Teenage boys get 44% of their 34 teaspoons of sugar a day from soft drinks. Teenage girls get 40% of their 24 teaspoons of sugar from soft drinks. The U.S. Department of Agriculture (USDA) recommends that people eating 2,200 calories a day not eat more than 12 teaspoons a day of refined sugar. Sugar consumption upsets the natural homeostasis of calcium and phosphorus in the blood. Normally, these minerals exist in a precise ratio of ten to four. The excess serum calcium, which comes from the bones and teeth, cannot be fully utilized because phosphorus levels are too low. Calcium is excreted in the urine or stored in abnormal deposits such as kidney stones and gallstones. High fructose corn syrup, which is the predominate sugar in soft drinks, inhibits copper metabolism. A deficiency in copper leads to bone fragility, as well as many other unwanted health conditions. Other research suggests that high fructose corn syrup, which has climbed from zero consumption in 1966 to 62.6 pounds per person in 2001, alters the magnesium balance in the body, which in turn accelerates bone loss. An optimal level of magnesium, which helps with calcium absorption, is essential for bone formation. Studies have found that magnesium deficiency is associated with osteoporosis and bone fragility. An adequate magnesium intake results in increased bone mineral density.
The latest government study shows a staggering 68% of Americans do not consume the recommended daily intake of magnesium. Even more frightening are data from this study showing that 19% of Americans do not consume even half of the government’s recommended daily intake of magnesium.
 In contrast to the normal nutrient-depleted “Western Diet,” research shows that consumption of fruits and vegetables, especially dark green leafy vegetables, offer considerable protection from osteoporosis. These foods are a rich source of bone-building vitamins and minerals and include calcium, magnesium, boron, and vitamin K. Vitamin K helps facilitate the production of osteocalcin, the major non-collagan protein in bone. Osteocalcin keeps calcium molecules anchored within bone. Boron supplementation has been shown to reduce urinary calcium excretion by 44 percent. It’s also required to activate certain important bone building hormones like vitamin D and 17-beta-estradiol, the most active form of estrogen.
In contrast to the normal nutrient-depleted “Western Diet,” research shows that consumption of fruits and vegetables, especially dark green leafy vegetables, offer considerable protection from osteoporosis. These foods are a rich source of bone-building vitamins and minerals and include calcium, magnesium, boron, and vitamin K. Vitamin K helps facilitate the production of osteocalcin, the major non-collagan protein in bone. Osteocalcin keeps calcium molecules anchored within bone. Boron supplementation has been shown to reduce urinary calcium excretion by 44 percent. It’s also required to activate certain important bone building hormones like vitamin D and 17-beta-estradiol, the most active form of estrogen.
Of course, most kids won’t go near a green leafy vegetable. And adults aren’t much better. Less than 10 percent of Americans eat the minimum recommendation of two fruits and vegetables a day. And worse, only 51 percent eat at least one vegetable a day.
So unfortunately, most folks are setting themselves up for trouble.
Calcium intake is the cornerstone for osteoporosis prevention.
Several studies have shown that calcium can reduce bone loss and suppress bone turnover. Calcium supplementation alone doesn’t halt bone loss completely but does reduce calcium excretion by 30-50 percent. One study shows that postmenopausal women taking one gram of elemental calcium were four and half times less likely to fracture than those on placebo.
The absorption of calcium is dependant on stomach acid for ionization. Because gastric acid facilitates the absorption of insoluble ingested calcium, stomach acid reducing drugs including Tums, Zantac, Nexium, Pepcid, Prilosec, and Tagament increase the risk of bone loss.
The hypochlorhydria (low stomach acid) produced by these drugs leads to decreased calcium absorption, thereby increasing bone loss and fracture risk. Similarly, proton pump inhibiting drugs (PPIs), like Prevacid, increase the risk of hip fracture. Studies show the risk of hip fracture is directly related to the duration of PPI use, ranging from 22% for 1 year of use to 59% for 4 years of use, relative to nonuse.
You should know that corticosteroids, and most diuretics (Lasix, Dyazide, Maxzide, and others) also deplete calcium.
Until recently, hormone replacement therapy was considered the best way to prevent bone loss and osteoporosis. And true, several studies have shown that estrogen replacement therapy can reduce bone loss and reduce the risk of fracture. However, the benefits have to be weighed against recent evidence linking conventional estrogen replacement therapy to increased risk of breast cancer, stroke, heart attack, and blood clots.
Another, certainly safer, option is to use phytoestrogens. Phytoestrogens are estrogen-like compounds found in certain foods including fennel, celery, soy, nuts, whole grains, apples, and alfalfa. A semi-synthetic isoflavanoid, known as ipriflavone, is similar in structure to soy and has been approved for osteoporosis prevention in Japan, Hungary, and Italy. Studies show that ipriflavone, now available as a supplement in the U.S., increases bone density in individuals with osteoporosis.
Several studies show that progesterone stimulates proliferation of bone building osteoblast cells. But, like synthetic estrogen, progestins (synthetic progesterone) are associated with numerous potentially dangerous side effects.
A natural over-the-counter form of progesterone can be made from wild yams. Based on the pioneering work of John Lee, M.D., compounded progesterone cream has been safely used by thousands of women to reduce or prevent menopause symptoms – and to reverse osteoporosis.
Vitamin D, a hormone-like substance, is crucial for the absorption of calcium. The skin makes Vitamin D after exposure to sunlight or ultraviolet radiation, and vitamin D deficiency is widespread throughout the United States. In the winter, vitamin D levels often plummet. Less than 10% of adults 50 to 70 years old, and only about 2% of people over 70, were found to be getting the recommended amounts of vitamin D from food. Even when supplements were added into consideration, still only about 30% of people aged 50 to 70, and 10% of those over 70 were reaching the recommended vitamin D intake.
Recommended Supplements