Fibromyalgia and Autoimmune Disease Is There A Connection?
Could fibromyalgia be due to an autoimmune disease?
New research suggests there may be an autoimmune reaction causing fibromyalgia symptoms.
Current estimates suggest that at least 1 in 40 people are affected by FMS worldwide (80% of which are women) and is commonly characterized by widespread pain throughout the body, as well as fatigue (often referred to as ‘fibro fog’) and emotional distress. It most commonly develops between the ages of 25 and 55, although children can also get it.

Those with fibromyalgia have numerous similar symptoms as those some common autoimmune diseases.
An Autoimmune disease has always been suspected, but never found. However, new research may be on to something.
New Fascinating Research Article
New research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London, in collaboration with the University of Liverpool and the Karolinska Institute, has shown some symptoms associated with fibromyalgia syndrome (FMS) are in fact caused by an autoimmune reaction.
The research shows that the autoimmune reaction is caused by antibodies that when triggered, increase the activity of pain-sensing nerves throughout the body.
Antibodies, also known as immunoglobulins, are proteins produced by the immune system in response to the presence of foreign substances, such as bacteria, viruses, or other pathogens.
Antibodies play a crucial role in the immune response by binding to specific antigens (molecules on the surface of pathogens) and marking them for destruction by other immune cells. This process helps the body to recognize and eliminate harmful invaders, protecting against infections and diseases.
Antibodies are produced by a type of white blood cell called B cells and come in various forms, each with specific functions in the immune system.
Autoimmune disease is a condition in which the immune system mistakenly attacks the body’s own cells and tissues. This can lead to inflammation and damage to various organs and tissues, causing a wide range of symptoms and health problems.
There are over 80 different autoimmune diseases, including rheumatoid arthritis, lupus, type 1 diabetes, and multiple sclerosis. Treatment for autoimmune diseases typically involves managing symptoms and suppressing the immune system to reduce inflammation and prevent further damage.
It’s not so far fetched. Could an autoimmune disorder be “the cause” of fibromyalgia?
The new research shows that fibromyalgia may be a disease of the immune system, rather than the currently held view that it originates in the brain.
The study, published today in the Journal of Clinical Investigation, demonstrates that the increased pain sensitivity, muscle weakness, reduced movement, and reduced number of small nerve-fibers in the skin that are typical of FMS, are all a consequence of patient antibodies.
“The implications of this study are profound. Establishing that fibromyalgia is an autoimmune disorder will transform how we view the condition and should pave the way for more effective treatments for the millions of people affected. Our work has uncovered a whole new area of therapeutic options and should give real hope to fibromyalgia patients.
Previous exploration of therapies has been hampered by our limited understanding of the illness. This should now change. Treatment for FMS is focussed on gentle aerobic exercises, as well as drug and psychological therapies designed to manage pain, although these have proven ineffective in most patients and have left behind an enormous unmet clinical need.”
Dr David Andersson, study primary investigator, King’s College London
Injected Mice Develop Fibromyalgia
The researchers injected mice with antibodies from people living with FMS and observed that the mice rapidly developed an increased sensitivity to pressure and cold, as well as displaying reduced movement grip strength.
In contrast, mice that were injected with antibodies from healthy people were unaffected, demonstrating that patient antibodies cause, or at least are a major contributor to the disease.
Furthermore, the mice injected with fibromyalgia antibodies recovered after a few weeks, when antibodies had been cleared from their system.
This finding strongly suggests that therapies, which reduce antibody levels in patients, are likely to be effective treatments.
Professor Camilla Svensson, the study’s primary investigator from Karolinska Institute said, “Antibodies from people with FMS living in two different countries, the UK and Sweden, gave similar results, which adds enormous strength to our findings.
The next step will be to identify what factors the symptom-inducing antibodies bind to. This will help us not only in terms of developing novel treatment strategies for FMS, but also of blood-based tests for diagnosis, which are missing today.”
‘Passive transfer of fibromyalgia symptoms from patients to mice’ Goebel et al https://doi.org/10.1172/JCI144201 is published in The Journal of Clinical Investigation
Research published in 2019 has already laid out the many factors fibro and autoimmune conditions they have in common including-
- They’re often triggered by trauma (stress) and infection.
- Various pathogens may increase the risk (Epstein-Barr virus, herpes simplex virus, hepatitis C).
- They can develop soon after vaccination, silicone breast implantation, or mineral oil injection.
- They’re more common in women.
- They involve genetic differences known to predispose you to autoimmunity.
Could Cell Danger Response Trigger An Autoimmune Reaction In Fibromyalgia? You bet it could!
The cell danger response (CDR) is a theory proposed by Dr. Robert Naviaux that suggests chronic illness, including autoimmune diseases, may be triggered by a persistent state of cellular stress and danger signaling.
According to this theory, various stressors, such as infections, toxins, or trauma, can disrupt cellular metabolism and communication, leading to a dysregulated immune response and the development of chronic health conditions.
While the exact relationship between the cell danger response and autoimmune diseases is still being studied, some researchers believe that prolonged activation of the immune system and cellular stress pathways could contribute to the development or exacerbation of autoimmune conditions.
Chronic inflammation and immune system dysfunction are common features of many autoimmune diseases, and it is possible that the cell danger response may play a role in perpetuating these processes.
The cell danger response (CDR) is a complex biological process that involves the activation of various signaling pathways and cellular mechanisms in response to stress or danger signals. Here are some key components and mechanisms involved in the cell danger response:
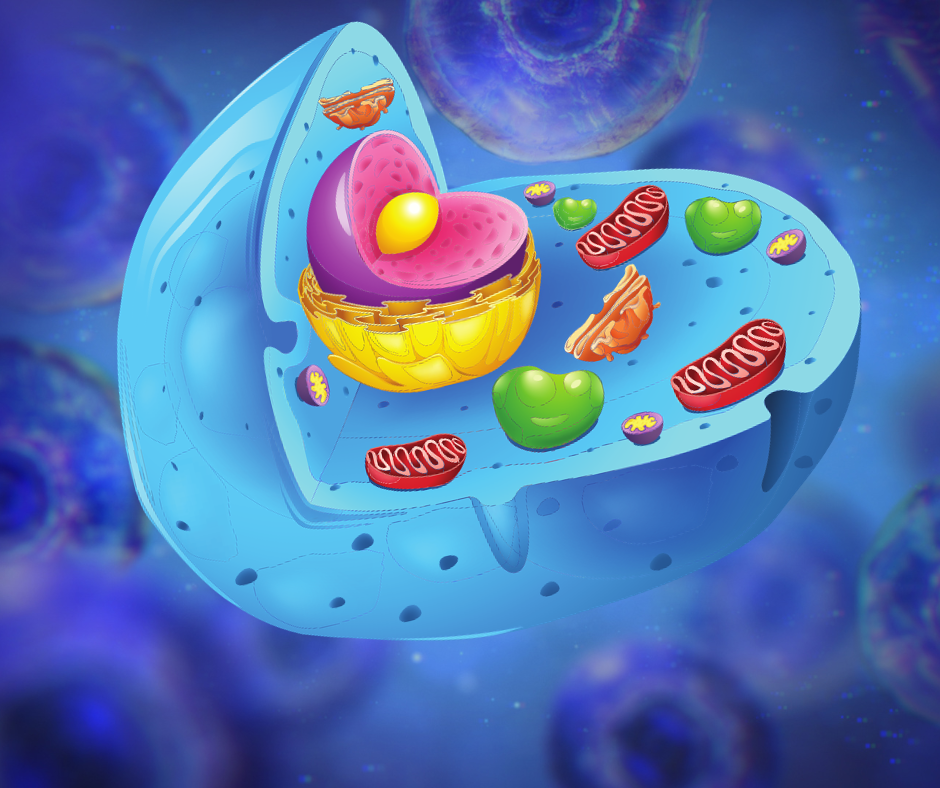
- Mitochondrial dysfunction: Mitochondria are the energy-producing organelles within cells, and they play a crucial role in cellular metabolism and signaling. During the cell danger response, mitochondrial function may be disrupted, leading to changes in energy production, oxidative stress, and the release of signaling molecules that can trigger immune responses.
- Inflammatory signaling: The cell danger response can activate inflammatory signaling pathways, such as the NF-kB pathway and the inflammasome, leading to the production of pro-inflammatory cytokines and chemokines. Chronic inflammation is a hallmark of many chronic diseases, including autoimmune disorders.
- Stress response pathways: Cells have evolved complex stress response pathways to cope with various environmental stressors. The cell danger response can activate stress response pathways, such as the unfolded protein response (UPR) and the heat shock response, to help cells adapt to and survive stressful conditions.
- Immune system activation: The cell danger response can trigger the activation of the immune system, leading to the production of antibodies, inflammatory mediators, and immune cells that can target and eliminate threats to the body. However, dysregulation of the immune response can also contribute to the development of autoimmune diseases.
- Metabolic changes: The cell danger response can lead to alterations in cellular metabolism, including changes in nutrient utilization, energy production, and redox balance. These metabolic changes can impact cell function and contribute to the development of chronic diseases.
Overall, the cell danger response is a complex and multifaceted process that involves the coordination of various cellular and molecular pathways to help cells adapt to and survive stressful conditions. Dysregulation of these mechanisms can contribute to the development of chronic illnesses, including autoimmune diseases.
Further research is needed to fully understand the mechanisms underlying the cell danger response and its implications for human health.
Read More About Cell Danger Response
P.S. Thanks to all who submitted new patient paperwork. Unfortunately, we’ve reached our limit and can’t accommodate everyone. Sorry, but Dr. Murphree isn’t accepting any more new patients at this time. If you want Dr. Murphree’s help please consider joining him and other members in the Fibromyalgia Rescue Group – Coaching Program.
Get the answers you need and the relief your looking for at: Endfibronow.com




Leave a Reply
Want to join the discussion?Feel free to contribute!