Are You Taking Lipitor, Zocor, Crestor or Stain Drug?
(updated February 2021)
If so you need to read this!
Are You Feeling Rundown? Has your Get Up and Go Got Up and Went?
 Over the last twenty years, the pharmaceutical companies have promoted cholesterol-lowering statin drugs with such fervor that they’ve become household names: Lipitor, Crestor, Vytorin, Zocor, and others. Accounting for 6.5% of the total market share, statin drugs are the most widely sold pharmaceutical drugs in history. To date, Forbes Magazine tells us that statins are earning drug companies $26 billion in annual sales. Pfizer spends over $3 billion each year to convince us that we need more and more drugs to be healthy. The public and the medical profession have been bamboozled by the legions of drug reps, billion dollar ad campaigns, and creative statistics.
Over the last twenty years, the pharmaceutical companies have promoted cholesterol-lowering statin drugs with such fervor that they’ve become household names: Lipitor, Crestor, Vytorin, Zocor, and others. Accounting for 6.5% of the total market share, statin drugs are the most widely sold pharmaceutical drugs in history. To date, Forbes Magazine tells us that statins are earning drug companies $26 billion in annual sales. Pfizer spends over $3 billion each year to convince us that we need more and more drugs to be healthy. The public and the medical profession have been bamboozled by the legions of drug reps, billion dollar ad campaigns, and creative statistics.
In 2004, Pfizer’s blockbuster drug Lipitor became the first prescription drug to make more than $10 billion in annual sales. Over twenty six million Americans have taken Lipitor, the most popular statin drug.
Every weekday, some 38,000 Pfizer sales reps, roughly the size of three army divisions, make their pitches around the globe. They’re armed with briefcases full of free drug samples, reams of manipulated clinical data, and lavish expense accounts for wining-and-dining doctors and their staff. The medical profession, its organizations, the media, and the public at large have swallowed the statin drug propaganda, hook, line and sinker.
Contrary to the Lipitor ads, apparently not, since a meta-analysis of 44 trials involving almost 10,000 patients showed the death rate was identical at 1 percent of patients in each of the three groups–those taking atorvastatin (Lipitor), those taking other statins and those taking nothing.
No doubt, the statins lower cholesterol levels and perhaps do lower the risk of dying from a heart attack–at least in patients who already have had one–but the size of the effect is unimpressive.
For instance, in one of the experiments, the CARE trial, the odds of escaping death from a heart attack in five years for a patient with manifest heart disease was 94.3 percent, which improved to 95.4 percent with statin treatment. This difference of 1.1 percent is surely not worth all the hype these medications have received, especially since the potential side effects from these drugs may include congestive heart failure.
And what about using statins as a prophylactic measure?
 A meta-analysis of 5 major statin drugs which showed that statin drugs provided a total absolute reduction in total mortality of 0.3% among those who showed no signs of having cardiovascular disease (primary prevention).
A meta-analysis of 5 major statin drugs which showed that statin drugs provided a total absolute reduction in total mortality of 0.3% among those who showed no signs of having cardiovascular disease (primary prevention).
The British Journal of Clinical Pharmacology reported on an analysis of all the major controlled trials before the year 2000 and found that long-term use of statins for primary prevention of heart disease produced a 1 percent greater risk of death over 10 years compared to a placebo.
A Denmark study that evaluated 500,000 patients found that taking statins for one year raised the risk of nerve damage by about 15%–about one case for every 2,200 patients. For those who took statins for two or more years, the additional risk rose to 26%.
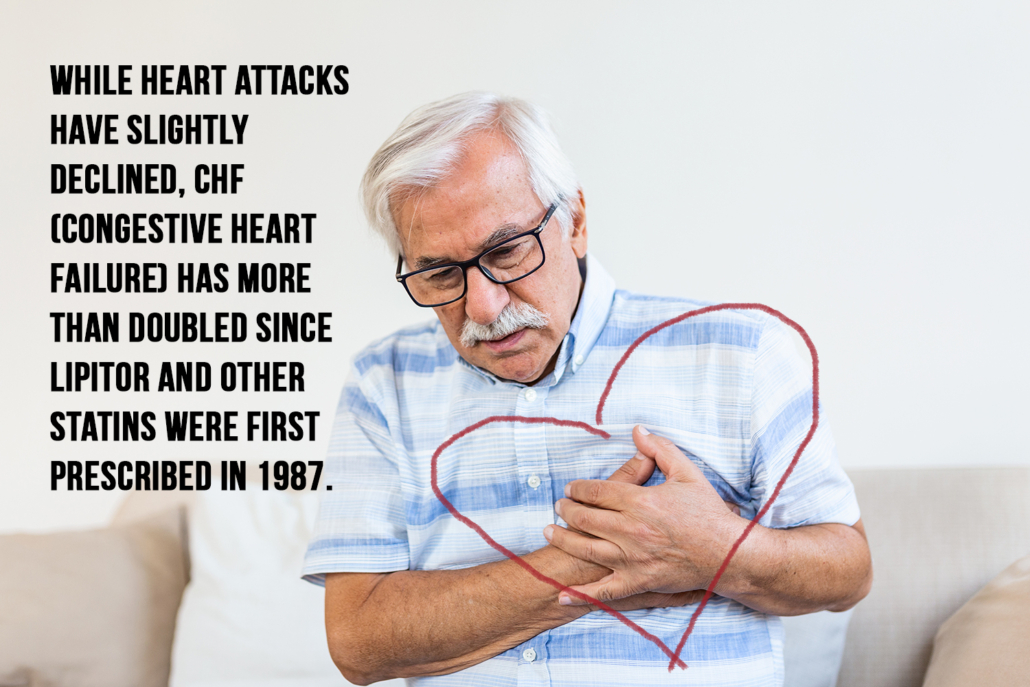
Former astronaut, Dr. Duane Graveline describes in his book, Lipitor: Thief of Memory, his complete memory loss due to the side effects of Lipitor. The incidence of congestive heart failure (CHF) has steadily increased since the introduction of statin drugs. In fact, while heart attacks have slightly declined, CHF has more than doubled since 1989. Statins were first prescribed in 1987.
An article published in the Journal of the American Medical Association reveals that in every study with rodents to date, statins have caused cancer. In the CARE trial, breast cancer rates of those taking a statin went up 1500%.
The only thing statin drug trials have proven for sure is that statin drugs lower cholesterol by inhibiting an enzyme known as HMG-CoA-Reductase. Regardless of their ability to lower cholesterol, they failed to show that this effect has any meaningful benefit for preventing early death from heart disease, heart attack or stroke.
And they’ve proven to be a catalyst for dangerous side effects. The most common side effect associated with statin drugs is muscle pain and weakness.
The symptoms are most likely due to the depletion of CoQ10, a nutrient that supports muscle function. One study found that 98% of patients taking Lipitor and one-third of the patients taking Mevachor (a lower-dose statin) suffered from muscle problems.
Interference with production of Co-Q10 by statin drugs is the most likely explanation. The heart is a muscle and it cannot work when deprived of the essential nutrient, Co-Q10. A deficiency of CoQ10 can lead to nerve damage and congestive heart failure.
Researchers studying CoQ10 have estimated that as little as a 25 percent reduction in bodily CoQ10 will trigger various disease processes, including high blood pressure, coronary artery disease, cancer, immune dysfunction, and fatigue
Don’t Take That Statin Without Taking CoQ10
 CoQ10 is also known as ubiquinone. It has been demonstrated that it is an essential nutrient for proper cardiovascular function. CoQ10 has been shown to be effective in returning heart function to normal. This is especially true when discussing congestive heart failure.
CoQ10 is also known as ubiquinone. It has been demonstrated that it is an essential nutrient for proper cardiovascular function. CoQ10 has been shown to be effective in returning heart function to normal. This is especially true when discussing congestive heart failure.
CoQ10 can’t be manufactured by the body. Instead, we must obtain CoQ10 from the foods we eat. Meat, dairy, and certain vegetables, such as spinach and broccoli, which contain the highest concentrations of CoQ10. We tend to absorb and utilize less CoQ10 as we age. Research also shows that we tend to need more CoQ10 as we age.
The primary function of CoQ10 is to provide cellular energy. In each cell there are organelles (small organ cells) known as mitochondria. They allow a chain of chemical reactions to create a spark, which generates 95 percent of the body’s energy. CoQ10 is the spark that helps ignite the energy production within the mitochondria. Without CoQ10 there is no cellular energy!
CoQ10 is more abundant in some cells and organs than in others. It tends to congregate in the organs, which need the most energy including the heart and liver. Researchers investigating CoQ10 have estimated that as little as a 25 percent reduction in bodily CoQ10 will trigger various disease processes including high blood pressure, coronary artery disease, cancer, and immune system dysfunction.
CoQ10 was discovered in 1957. Dr. Karl Folkers and fellow researchers at the University of Texas in Austin are credited with identifying the importance of CoQ10 in bodily functions. Dr. Folkers has been honored with the Priestly Medal, the highest award bestowed by the American Chemical Society, for his work with CoQ10, vitamins B6, and B12. In his acceptance for the Priestly Medal, Dr. Folkers pointed out that CoQ10 therapy was a major advancement in the treatment of heart disease. In fact, one of the studies he sited showed that the those treated over a 3 year period with CoQ10 and conventional medical therapies had a 75 percent survival rate compared to a 25 percent survival rate for those who used conventional drug therapy alone. Dr. Folkers went on to say, “I believe it is quite possible that cardiovascular disease may be significantly caused by a deficiency of CoQ10.”
The results of using CoQ10 in treating heart disease can be quite dramatic as the study below illustrates.
A group of class IV (terminal) congestive heart failure patients were supplemented with CoQ10 in addition to their prescription medications. Normally, class IV patients live only a matter of days. Seventy one percent of those taking the CoQ10 survived one year and 62 percent survived 2 years!
Several studies have demonstrated the role high blood pressure plays in heart disease. Research also shows that CoQ10 is able to reduce blood pressure in high-risk heart disease patients. In one study CoQ10 lowered systolic pressure from an average of 141 to 126 and diastolic from 97 to 90.
CoQ10, until recently, was a prescription medication in Japan. It is quite popular in Japan where there hundreds of commercial CoQ10 preparations from more than 80 different pharmaceutical companies.
 Over 12 million (approximately 10 percent of the population) Japanese take CoQ10 on a regular basis to prevent and treat heart disease. This number is rapidly growing since the recent change in laws that now allow CoQ10 to be sold over the counter. Japanese physicians have a long track record of using CoQ10. In fact, 75 percent of all supplemental CoQ10 comes from Japan. The popularity of CoQ10 has made the price of the high quality Japanese CoQ10 which reaches the United States, fairly expensive. Venders and manufacturers say the price will eventually come down once the large Japanese manufacturers increase the capacity to meet the growing demand for CoQ10.
Over 12 million (approximately 10 percent of the population) Japanese take CoQ10 on a regular basis to prevent and treat heart disease. This number is rapidly growing since the recent change in laws that now allow CoQ10 to be sold over the counter. Japanese physicians have a long track record of using CoQ10. In fact, 75 percent of all supplemental CoQ10 comes from Japan. The popularity of CoQ10 has made the price of the high quality Japanese CoQ10 which reaches the United States, fairly expensive. Venders and manufacturers say the price will eventually come down once the large Japanese manufacturers increase the capacity to meet the growing demand for CoQ10.
Dosage?
I recommend my patients consider taking a minimum of 100-200 mg for prevention and treatment of coronary heart disease, including associated high blood pressure.
–> Learn More About Essential Therapeutics CoQ10
Learn the truth about cholesterol, heart disease, and CoQ10 by reading my book, “Heart Disease What Your Doctor Won’t Tell You.”
(update)
A study, which tracked individuals over the course of six years, determined that using cholesterol lowering drugs (otherwise known as statins) as a primary method of preventing cardiovascular disease puts individuals at an increased risk for developing diabetes and other complications.
The risk of developing diabetes from using statins has been documented. What has not been documented is the risk of developing diabetic complications as a result. The findings of Ishak Mansi, M.D., from the Veteran’s Affairs North Texas System, department of medicine were published in the Journal of General Internal Medicine.
It was remarked in this publication that this study is among the first to show the correlation between diabetes and statins in individuals that are otherwise healthy. Previously conducted studies showed a connection between statin use and diabetes, but only in individuals who already had a greater medical risk.
Further research must be conducted in order to assess the risk over longer and shorter periods of use.
 The study did, however, confirm that patients who were taking statins were more likely to develop either diabetes and/or pre-diabetes. Those who developed diabetes had more complication related to their diabetes, but it is not clear if these enhanced complications were more a result of statin use or if these complications were a result of factors which exist within that population (diet, genetics, environment, etc…).
The study did, however, confirm that patients who were taking statins were more likely to develop either diabetes and/or pre-diabetes. Those who developed diabetes had more complication related to their diabetes, but it is not clear if these enhanced complications were more a result of statin use or if these complications were a result of factors which exist within that population (diet, genetics, environment, etc…).
The use of statins is not beneficial for everyone and their use needs to be minimal in the medical community. Women, for example, are at a lower risk of getting cardiovascular disease than men are and can be put on heart-friendly diets in lieu of medications like statins.
Doctors who regularly prescribe statins maintain that the benefits far outweigh the risks involved, especially when it comes to second level prevention. The long-term effects of using statins as a primary prevention method have not been thoroughly studied.
Between October 1, 2003, and March 1, 2012, a group of individuals were divided into those who used statins (primarily as Simvastatin) and those who did not. All individuals who had diabetes, cardiovascular disease, or a life-limiting chronic condition were excluded from the study. Using a checklist of 42 baseline characteristics, researchers were able to generate a balance of statin and non-statin users.
Approximately 14% of the total patients developed diabetes, which is along the National Average. The part that was not average was the amount of statins users who had to make more visits to the doctor’s office for medical issues.
After compounding the data, the researchers determined that those patients taking statins had an 85% higher risk of developing diabetes. They also had twice the risk of developing complications from diabetes and an increased risk of obesity when compared to non-statin users.
The debate still goes on.
If you’re taking a statin medication, I recommend you add 200mg of CoQ10 a day to your diet.





Leave a Reply
Want to join the discussion?Feel free to contribute!