This theory helps explain why someone gets fibromyalgia and other chronic illnesses
Cell Danger Response Theory (excerpt from upcoming 6th edition Dr. Murphree’s “Treating and Beating Fibromyalgia” book).
Dr Robert Naviaux professor of Medicine, Pediatrics and Pathology at UC San Diego School of Medicine, published “Metabolic Features of the Cell Danger Response (CDR)” in 2014. This study outlined the cellular response to chemical, physical and biological threats. His research is a game changer for doctors and their patients. Dr. Naviaux explains CDR:
“In chronic illness, the original triggering event is often remote, and may no longer be present. Emerging evidence shows that most chronic illness is caused by the biological reaction to an injury, and not the initial injury or the agent of injury itself. For example, melanoma can be caused by sun exposure that occurred decades earlier, and post- traumatic stress disorder (PTSD) can occur months or years after a bullet wound has healed. If healing is incomplete between injuries, more severe disease is produced. Chronic disease then results when cells are caught in a repeating loop of incomplete recovery and re-injury, unable to fully heal. This biology is at the root of virtually every known chronic illness, including susceptibility to sequential or recurrent infections, autoimmune diseases like rheumatoid arthritis, diabetic heart and kidney disease, asthma, and chronic obstructive pulmonary disease (COPD), autism spectrum disorder (ASD), chronic fatigue syndrome (CFS), cancer, affective disorders, psychiatric illnesses, Alzheimer dementia, and many more.”
 Cell Danger Response, or CDR is essentially the body’s response to any perceived threat, real or imagined.
Cell Danger Response, or CDR is essentially the body’s response to any perceived threat, real or imagined.
Stress, an infection or illness, or an encounter with environmental toxins can trigger cell danger response. A complete CDR cycle in the body starts with a “stressor” and ends with recovery.
Factors that may trigger the CDR include:
- Biological stressors, such as viruses, bacteria, parasites, and fungi, as well as nutrient deficiency, nutrient depletion, hypoxia or low oxygen, inflammation, or oxidative stress.
- Chemical stressors, such as heavy metal toxicity, chemical toxins, other toxins, and medications.
- Physical stressors and trauma, such as accidents, injuries, burns, surgeries, and major infections.
- Psychological stressors or trauma, such as divorce, loss of a loved one, emotional neglect, emotional abuse, major financial difficulties, and dealing with a chronic disease.
A case of influenza or “flu,” is a good example of CDR in action. Once exposed to the virus, your body initiates CDR. Over the course of several days you may experience aches, all over pain, fatigue, brain fog, GI symptoms, and poor sleep. Eventually, after doing it’s job – fighting off the virus, the CDR is turned off, the healing cycle is complete and your symptoms disappear.
The CDR response is meant to be short-term.
However, when the body undergoes chronic stress from ongoing bacterial, fungal, parasitic infections, poor sleep, heavy metals, and or toxins, the ‘danger response’ may become stuck, causing your body to remain in a chronic defensive posture.
CDR helps answer some of the questions as to why some people get sick and stay sick while others make a full recovery.
Symptoms that you might experience with a prolonged or “stuck” healing response include the following:
- Fatigue
- Chronic pain and inflammation
- GI issues, bloating, gas, pain, irritable bowel
- Poor sleep
- Depression
- Brain fog/poor memory
- Poor exercise tolerance and a decreased ability to recover after exercise
- Inflammation, edema, swelling
- Rashes
Your Mighty Mitochondria
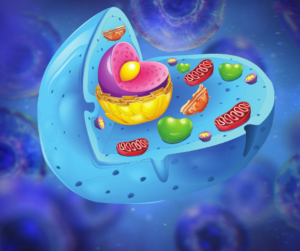
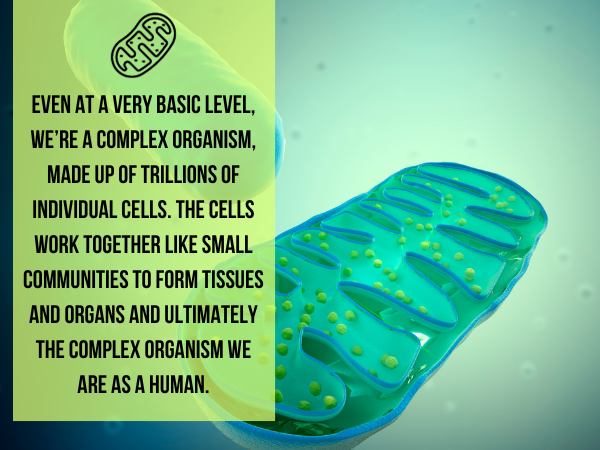
Within each individual cell are many components, including the mitochondria, the power plants of the cell. Mitochondria produce energy– adenosine triphosphate (ATP), from the food we consume to power our cells, tissues and organs. Everything from your heartbeat to your muscle movements depends on an adequate supply of adenosine triphosphate (ATP) being generated by the mitochondria. These organelles are responsible for producing about 40% – 100% of your body weight in ATP every single day.
In an acute stress situation, the body’s mitochondria increase their production of adenosine triphosphate or ATP (energy) and then after the danger is eliminated, stimulate anti-inflammatory, regenerative pathways to restore healing.
Most cells have between 1,000 and 10,000 mitochondria per cell. The most important cells have the highest concentrations, with the eyes, brain, and heart containing around 10,000 mitochondria per cell, and the liver containing around 2,000 per cell.
Some scientists estimate that the mitochondria in the human body collectively house as much potential energy as a lightning bolt! Mitochondria have an electric field strength of 30 million volts, which is equivalent to a lightning bolt… or 2.5 million car batteries.
Unfortunately, research has shown that in people with fibromyalgia, cells have fewer mitochondria and the mitochondria that are present, often don’t function properly, compared to healthy controls. This may be due to a genetic abnormality, nutrient deficiencies, oxidative stress, or a combination of these factors. Regardless, it puts those with fibromyalgia at a distinct disadvantage.
Our cells must maintain a certain level of energy to maintain balance (cellular homeostasis). There is a minimum level of energy required at any given time to maintain the day-to-day functions of the cell. If there is a significant drop in energy below a specific threshold, the mitochondria will sense this drop of energy as a threat. As a result, the mitochondria will change their primary function from energy production to cell defense.
A stressed cell that meets with a toxin or pathogen will begin to leak ATP into the bloodstream. It is this extracellular ATP (which under normal circumstances is found only inside of the cell) that initiates the first phase of cell danger response. Eventually, the mitochondria shuts down energy production and scrambles outside of the cell to signal the immune system. This in turn triggers inflammation.
Hormone production and communication may be compromised from CDR.
This is one reason why hormonal problems are so common in those with chronic illness, including those with fibromyalgia who often struggle with low cortisol, DHEA, neurotransmitters (serotonin, dopamine, norepinephrine), and thyroid hormones.
Hormones also work to regulate mitochondrial function. Thus, if hormone levels are off, it will impair mitochondria, which will further impair hormone production.
The mitochondria also have two-way communication with the nervous system. If mitochondria sense danger they will communicate to the nervous system and signal to make alterations. Likewise, if the nervous system is under duress, it will also communicate to the mitochondria to begin the transition into CDR.
This relationship is especially true for mitochondria and the vagus nerve. The vagus nerve starts in the brain and then extends downward into the lungs, heart, and intestines, as well as into several muscles. It has a physical effect on swallowing, sweating, digestion, speech, and heart rate, among other bodily functions.
Notably, the vagus nerve is also highly integrated into the parasympathetic branch of the nervous system, which is a network of nerves that relaxes your body in response to danger or stress. It’s associated with the “rest and digest” responses, whereas the sympathetic branch of the nervous system deals with the “fight or flight” response. Another chapter, those with fibromyalgia are typically stuck in a hyper vigilant, over aggressive sympathetic state, creating cellular stress and Central Sensitization Syndrome (CNS).
CNS intensifies nerve signals, causing a person to have more intense sensory experiences than usual. This often results in chronic pain and negative reactions to stress and stimulation (touch, loud noises, bright lights, odors, etc).
An under stimulated vagus nerve, common in those with central sensitization pain syndrome, including fibromyalgia patients, can result in lower mitochondrial function. Vagal stimulation exercises can be extremely helpful in reducing cell danger response, overall stress and in generating more energy boosting mitochondria.
Supporting mitochondria is crucial for managing chronic illness.
Here are some tips for stimulating your vagus nerve to produce more mitochondria:
Chanting, humming, singing, talking, and other vocal chord exercises to increase heart rate variability
EPA and DHA found in seafood and fish and or krill oil supplements.
Meditating not only boosts mood and lowers anxiety, but also increases vagus nerve and parasympathetic system activity.
Research shows social relationships make individuals feel closer to others, and that feeling stimulates the vagus nerve.
Chewing gum boosts the release of the hormone, CCK, from the gut, which helps facilitate communication from the vagus nerve to the brain.
Fiber increases GLP-1, a hormone that supports communication between the vagus nerve and brain.
Exercise stimulates the vagus nerve.
Intermittent fasting reduces the number of calories consumed. That reduction in calories causes heart rate variability to spike and metabolism to plummet—two events that trigger vagus nerve function.
Acupuncture, especially to the ear, stimulates the vagus nerve.
Sunlight–UVA rays increase the body’s levels of melanocyte stimulating hormone (MSH), another hormone that stimulates the vagus nerve.
Studies show praying stimulates the vagus nerve by increasing diastolic blood pressure and heart rate variability.
Temperatures colder than average body temperature triggers the parasympathetic nervous system into action. Drinking cold water, dipping your face in cold water, or taking cold showers stimulates the vagus nerve.
Whole body, neck and foot massages stimulate the vagus nerve.
Serotonin activates the vagus nerve through several different receptors in the body.
Research confirms that pulsed electromagnetic field therapy (PEMF) stimulate the vagus nerve by increasing heart rate variability.
How Do You Turn Off CDR
The cell danger response is not something that can be simply turned off. However, addressing the underlying causes of cellular stress, such as reducing inflammation, managing oxidative stress, and promoting overall cellular health, may help regulate the cell danger response. This can be achieved through various lifestyle factors, including a balanced diet, regular exercise, stress management techniques, and adequate sleep. Here is a three-pronged approach for overcoming a “stuck” cell danger response.
- First remove any triggers that initiate Cell Danger Response-toxins, pathogens, and chronic stress. Tests can show if you have mold, Lyme, heavy metals, parasites, food allergies, or opportunistic pathogens (parasites, Candia, viruses, etc). Find them and eliminate them.
- Support mitochondrial function so that they navigate the CDR process efficiently (see above list).
Magnesium is also critical for our mitochondria to produce energy. Magnesium gets depleted rapidly when we are exposed to oxidative stress which we are all chronically exposed to. We can find this nutrient abundant in dark leafy vegetables, seeds, nuts, legumes, seafood and organic chocolate.
However, those under chronic stress (most everyone), or those chronically ill, will need to supplement with magnesium to ensure we are getting adequate amounts.
B vitamins, carnitine, vitamin C, and selenium, are also very supportive to our mitochondria. We can acquire these nutrients from foods like seeds, seeds, citrus fruits, fish, and meat.
Eating an anti-inflammatory diet is one of the easiest ways to improve mitochondrial function. Polyphenol-rich foods are high in healthy mitochondrial-boosting polyphenols.

Using intermittent fasting methods such as timed eating and intermittently “going keto” are also mitochondrial boosters.
Nutrients Needed For Optimal Mitochondria Function
Co-Q 10 is an essential electron carrier in the mitochondrial respiratory chain and needed for optimal mitochondria function. If you have a chronic illness, especially fibromyalgia, I believe this enzyme should be taken on a daily basis. I put all my patients on the Fibromyalgia Formula multivitamin mineral formula with CoQ10.
Alpha-lipoic Acid is a potent fat and water-soluble antioxidant vitamin. It is also a metal chelator (helping to remove iron, copper, mercury, and other heavy metals). It acts as an anti-inflammatory supplement.
Acetyl-l-Carnitine is a naturally occurring fatty acid transporting amino acids. L-carnitine supplementation has long been studied and then used in many mitochondrial dysfunction disorders.
 These disorders are also characterized by low concentrations of serum l-carnitine levels as seen in heart disease, diabetes, kidney disease, and chronic overwhelming infections. An important cellular longevity function of l-carnitine has been to increase the rate of mitochondrial oxidative phosphorylation (ATP production) that declines with age.
These disorders are also characterized by low concentrations of serum l-carnitine levels as seen in heart disease, diabetes, kidney disease, and chronic overwhelming infections. An important cellular longevity function of l-carnitine has been to increase the rate of mitochondrial oxidative phosphorylation (ATP production) that declines with age.
NAC-Studies are increasingly showing that mitochondrial illnesses are fueled by oxidative stress, implicating the use of antioxidants such as natural vitamin E and NAC (the precursor to glutathione) as well as glutathione.
Glutathione is a tri-peptide made up of the amino acids: cysteine, glycine, and glutamic acid. It is known as the master antioxidant in the body.
Liposomal glutathione refers to glutathione that has undergone a special process that encapsulates the glutathione molecule inside of a lipid. Doing this protects the glutathione molecule and dramatically improves absorption. Glutathione is primarily produced by our cells, though as we age, our bodies produce less and less.
While a small amount of glutathione is available in certain foods, such as spinach, avocado, and asparagus, a high-quality, clinically researched liposomal glutathione supplement is the best way to increase glutathione within the body. An imbalance of free radicals and antioxidants can cause oxidative stress.
Oxidative stress can cause chronic inflammation. Infections and injuries trigger the body’s immune response. Immune cells called macrophages produce free radicals while fighting off invading germs. These free radicals can damage healthy cells, leading to inflammation. Under normal circumstances, inflammation goes away after the immune system eliminates the infection or repairs the damaged tissue.
However, oxidative stress can also trigger the inflammatory response, which, in turn, produces more free radicals that can lead to further oxidative stress, creating a cycle. Chronic inflammation due to oxidative stress may lead to several conditions, including fibromyalgia, diabetes, Alzheimer’s, Parkinson’s, cardiovascular disease, and arthritis.
De-stress and give your body permission to heal
Reestablishing consistent deep restorative sleep, cleaning up your diet, environmental exposure, meditation, prayer, quite time, yoga, gardening, massage, nature walks, and other stress reducing activities help give your body permission to turn off CDR and complete the healing cycle.
Cell danger response is a fascinating, paradigm shifting theory that is changing the way we look at and treat chronic illness. Rather than blaming the symptom(s), patient, or past trigger(s) for a chronic disease, the focus should be on how to help the individual and their cells, complete the healing cycle.
I believe functional medicine, which focuses on finding and fixing root causes and treating the whole person rather than suppressing symptoms, is uniquely positioned to embrace and harness the Cell Danger Response. I encourage you to work with a functional medicine practitioner who specializes in Fibromyalgia. In the meantime, start applying some of these self-help ideas. Give yourself (and your cells) permission to feel safe. Complete the Cell Danger Response and begin to feel good again.




Very good information.
Please sign me up to receive your Blogs.
Thank you!